A 47-year-old man presented complaining of gradually decreasing vision and monocular diplopia in his right eye for approximately the past 18 months. He had undergone LASIK vision correction over 13 years earlier with an excellent emmetropic outcome. His prior prescription was a spherical equivalent of about (-) 10.00 DS in each eye. At this point, his best acuity is 20/70 OD and 20/20 OS. He had been to several eye care practitioners in recent months with no identified reason for the vision decrease. Results of perimetry, pupil testing, macular OCT, biomicroscopic and fundus evaluation, pachymetry, and corneal topography were all reportedly normal.
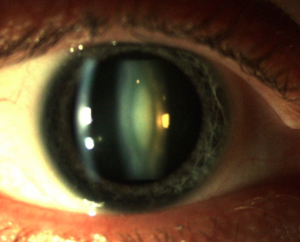
The key diagnostic findings included a pinhole improvement to a crisp 20/25 acuity though he refracted no better than 20/70. Most telling was a refractive shift of (-) 4.50 diopters. Now, a careful lens evaluation revealed a dense, “milky” nuclear opalescent cataract in the right eye only.
Patients typically develop “milky” nuclear sclerotic cataracts at an earlier age than other forms of lens opacification. The onset is often unilateral or asymmetric, usually developing during middle age, often beginning in the 40s and 50s. Males are often more affected than females and patients are typically moderately to highly myopic.
Patients will often complain of declining vision which is more rapid than with other types of cataract. Monocular diplopia occurs commonly though most patients will describe it as blurred vision. Pinhole testing relieves monocular diplopia and may significantly improve vision, though the patient may not see similar improvement with subsequent refraction. Patients will commonly have a myopic shift that can be relatively dramatic, accounting for up to 1-2 diopters per year. As the myopia is refractively corrected, best visual acuity declines to a point where the patient cannot tolerate the spectacle imbalance, visual acuity, or both.
In contrast to generalized cataractogenesis, there will be a white density within the nuclear core that is best appreciated with a fine biomicroscopic slit beam (optic section) directed off the visual axis. Comparison to the fellow eye in unilateral or asymmetric cases is often helpful in making the diagnosis, which may be subtle. Also in contrast to other types of cataracts, patients can present with significantly reduced vision, yet the funduscopic view is minimally altered; that is, practitioners will have a clear view into the eye yet the patient reports poor visual acuity. When this occurs, diagnosing cataract is not intuitive and the patient may go through additional testing and referral needlessly. Ultimately, the patient successfully underwent cataract extraction with an excellent outcome.
When encountering such a clinical situation, remember the M-Rule: Myopic, Male, Middle-aged, Myopic shift, Monocular diplopia, Milky nucleus