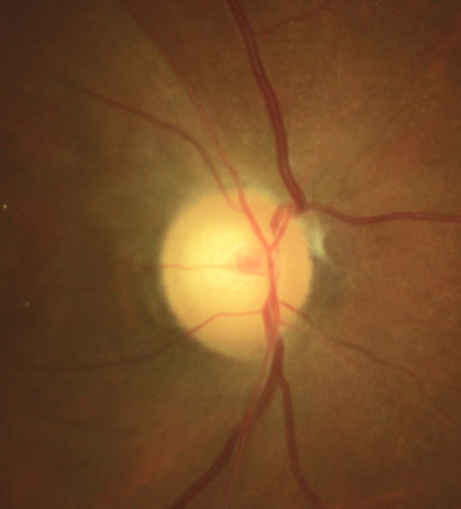
 A 46-year-old woman presented for a scheduled IOP check and visual field as a glaucoma suspect. She had a history of breast cancer 5 years earlier and was using tamoxifen. She reported that she got some cleaning fluid in her right eye 4 weeks earlier. She said that she had some moderate pain and visual blur which subsided, but then several hours later her vision significantly diminished in this eye. She attributed this to the chemical getting in her eye. She did not seek any care and reported that she felt her vision had improved, despite the fact that she was now 20/400 OD (previously she was 20/20). She now had a prominent relative afferent pupil defect OD. Biomicroscopy was normal and showed no chemical injury. Fundus examination revealed a pale optic disc with attenuated retinal arterioles and optical coherence tomography showed profound retinal thinning. Previous disc photos showed a pink and perfused nerve and normal vasculature.
A 46-year-old woman presented for a scheduled IOP check and visual field as a glaucoma suspect. She had a history of breast cancer 5 years earlier and was using tamoxifen. She reported that she got some cleaning fluid in her right eye 4 weeks earlier. She said that she had some moderate pain and visual blur which subsided, but then several hours later her vision significantly diminished in this eye. She attributed this to the chemical getting in her eye. She did not seek any care and reported that she felt her vision had improved, despite the fact that she was now 20/400 OD (previously she was 20/20). She now had a prominent relative afferent pupil defect OD. Biomicroscopy was normal and showed no chemical injury. Fundus examination revealed a pale optic disc with attenuated retinal arterioles and optical coherence tomography showed profound retinal thinning. Previous disc photos showed a pink and perfused nerve and normal vasculature.
Based upon her history of sudden, painless vision loss, a pale disc, attenuated retinal vessels, and profound retinal thinning on OCT, she was diagnosed with a central retinal artery occlusion (CRAO). The chemical exposure had no bearing.
The epidemiology of CRAO varies with systemic diseases and risk factors that cause them such as heart disease, cardiovascular disease, giant cell arteritis, smoking, obesity and other chronic or episodic contributors such as bacterial endocarditis. Emboli from various sources travel through the vascular system becoming lodged inside the central retinal artery obstructing the flow of blood to distal tissues. Calcific emboli are most likely to cause retinal artery occlusion and are often cardiac in origin. Etiologies related to malfunctioning clotting factors in blood such as antiphospholipid disease, factor VIII abnormality along with protein S and C alteration are also possible etiologies.
In a 46-year-old patient, conditions such as giant cell arteritis, atherosclerosis, hypertension and diabetes are typically not responsible for CRAO and alternate etiologies should be sought. Tamoxifen is a selective estrogen receptor modulator widely used in the treatment of hormone-responsive breast cancer. Tamoxifen has been noted to cause a crystalline retinopathy and should be in the differential of possible causes. However, this patient had a unilateral occurrence and no crystalline maculopathy, thus a direct cause is unlikely.
An association of tamoxifen with large vessel thromboembolic events (especially venous thrombosis) has been established. CRAO can be caused by inherited or acquired thrombophilia, especially homocysteinemia. Thrombophilia is also caused by exogenous estrogens, estrogen progestin oral contraceptives, clomiphene citrate, and selective estrogen receptor modulators (such as tamoxifen). Additionally, malignancies such as breast cancer create a pro-thrombotic state with an increased risk of thromboembolism.
This patient was in 5-year remission for breast cancer. In the absence of other potential etiologies, it was determined that tamoxifen-associated thrombophilia likely precipitated her CRAO. As the occlusion was over a month old, urgent referral to a stroke unit stroke was not required. Communication was made with the patient’s primary care physician to inform of the retinal vascular event and initiate investigation for a pro-thrombotic state and discuss the possible association with tamoxifen use and prevention of future thrombotic events.
This comment relates to Case Challenge 10, thx for an interesting case, one that I agree is atypical, and likely points to an atypical etiology.
re: sources of emboli, I was under the impression that retinal emboli were more typically of carotid origin, whereas cardiac valve/aortic arch disease and atrial fibrillation were more likely to cause cerebral ischemia.
Appreciate the effort they goes into preparing these cases. Thx again.
Derek, our pleasure to supply the cases. Thanks for reviewing them and the comments! Watch for more cases.